How I Fixed Foot Swelling
Here's the story of how I fixed foot swelling (lower limb edema) by changing my diet.
It was simple but not easy. I had to eat crow, as they say; not literally, but metaphorically.
I took the below photo of my lower limb edema on August 8, 2021 at 9:10:52 PM.

My feet were not only swollen, they were cold, even in the middle of August, indicating that I had impaired blood circulation to and from the feet.
I fixed this problem over the course of a year using dietary changes. I took the following photo of my feet on August 7, 2022 at 9:27:25 PM.

I took both photos on a Sunday night after I had spent the entire afternoon sedentary, deterred from outdoor physical activity by high temperatures and humidity with a high heat index in lower Michigan
Once I finally figured out how to fix lower limb edema, it took just a couple of months of consistent dietary change to get this result.
My Foot Swelling Story
I had started having this foot swelling problem during 2019, which was two years after I had adopted a hypercarnivore diet, and the year after I published The Hypercarnivore Diet, which was my attempt to summarize evidence that I construed to be supportive of consumption of a diet providing more than 70% of energy from animal products.
This illustrates how it can take months or years for the adverse effects of an unhealthy diet to manifest. In late 2017, several months after adopting the high fat meat-based diet, I had been able to rationalize my potentially harmful very high cholesterol levels with the "lean mass hyper-responder" hypothesis, because I had no externally visible signs of impaired health. In contrast, in 2019, after nearly 2 years eating a hypercarnivore diet, I could not ignore this foot swelling, a clear sign of impaired circulation and health.
When the lower limb edema first occurred I was attempting a very high fat, very low carbohydrate, restricted protein ketogenic iteration of hypercarnivore (similar to the so-called 'paleolithic ketogenic diet'), to find out if this would improve my scalp psoriasis, which had barely responded (if at all) to the hypercarnivore approach. To get a very high fat and lower protein intake I was eating more fatty animal foods, including salty bacon and hard cheese, and to reduce carbohydrate and protein, I was avoiding milk, yogurt and lean meat. Consequently, I ended up with a low potassium intake as well (animal fat supplies no potassium, cheese has much less potassium than milk or yogurt).
Before the cold feet and foot swelling became a very noticable issue, I was plagued with severe muscle cramping that started with cramps in my shins and feet waking me up from sleep. To limit protein and carbohydrate intake, I tried to fix the cramping problem by eating more salt and drinking more water, as suggested by the low-carbohydrate advocates.
That didn't work. I went from having lower limb cramping only at night to lower limb cramping during the day, particularly in the morning during my strength training sessions. Next came severe cramps in my abdominal muscles during strength training sessions. Soon I was getting cramps in my feet, legs and abdomen when seeing patients in my acupuncture practice.
I knew that cramping was a sign of potassium deficiency but in order to sustain the very low carbohydrate and moderate adequate protein intake I could not eat high potassium foods. The alleged remedy for cramping recommended by leading advocates of low carbohydrate diets––eating more salt and drinking more water––didn't reduce my cramps, but it did result in me having cold feet and foot swelling (lower limb edema) many nights before bed.
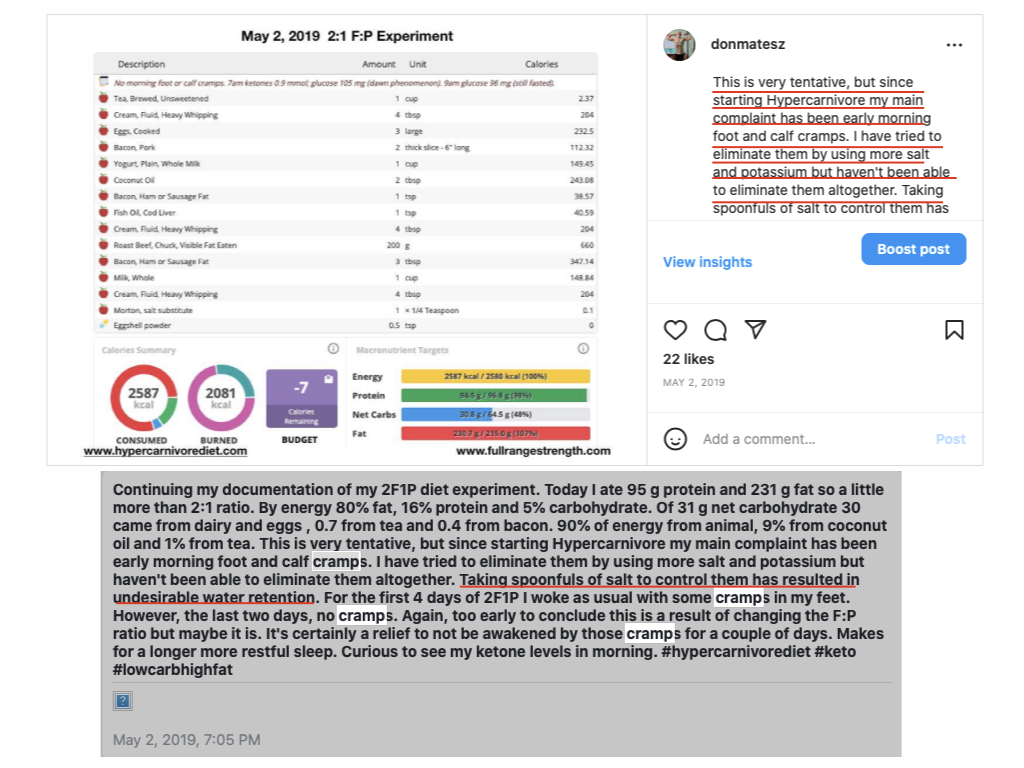
Although I had relief from the cramps during the first week on the higher fat, lower protein diet, they then returned with a vengeance. So long as I remained on the low carbohydrate hypercarnivore diet the condition continued to worsen. Eventually I was having cramps in my pectorals, thighs and biceps.
Eventually I had to accept that I could not continue with the high sodium:potassium ratio of the very low carbohydrate diet. In addition to reducing sodium intake, I had two choices: use potassium supplements or add potassium-rich foods back into my diet. I opted for the latter. I reduced my animal fat intake, increased milk products and lean meats (higher in potassium than fatty meats), and added fruits (whole and juices) back into my diet.
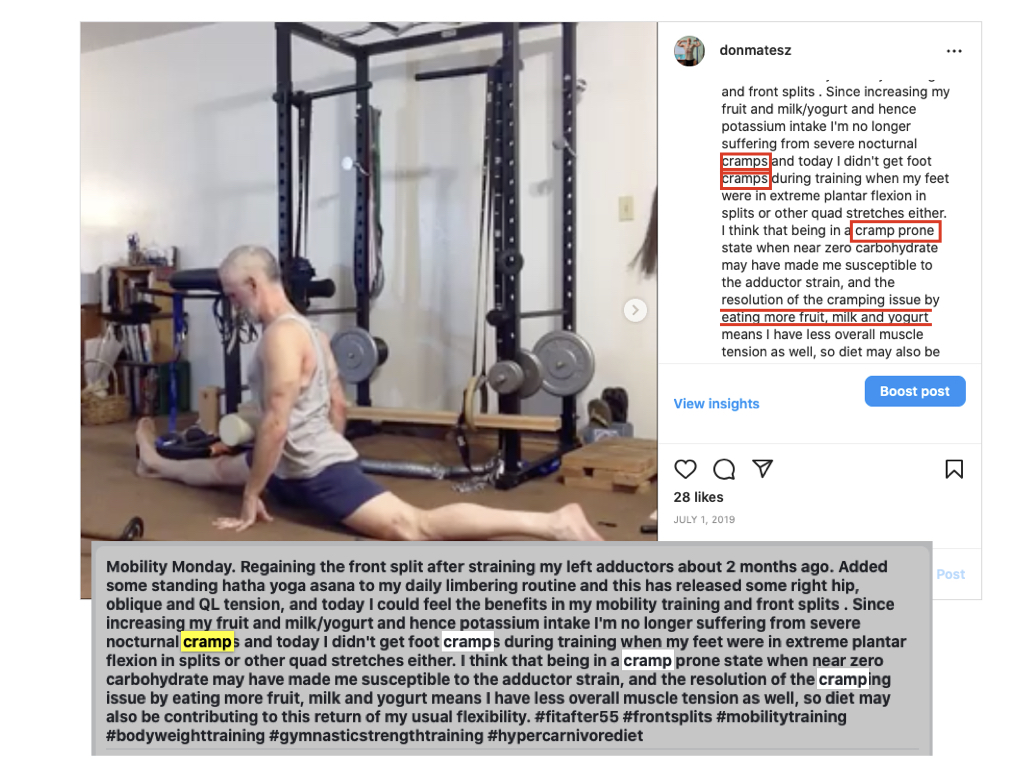
This readily resolved the cramping issue, and over 2019-mid2021 I used the "meats and sweets" dietary approach. During this phase I gradually found that the psoriasis type lesions in my ears improved the most when I obtained most of my calories from dairy products and fruits and reduced my intake of fatty meats, particularly beef, in favor of leaner meats in smaller portions.
However, although this change did resolve the cramping and, in combination with supplements and herbs, greatly improved the psoriasis in my ears, it didn't have much impact on the psoriasis on my scalp and did not correct the foot swelling issue. In fact, the initially intermittent foot swelling problem gradually became more persistent.
In August 2021, after I took the lead photo in this article, I decided I needed to make more significant changes to my diet. Since the foot swelling problem started when I started increasing salt intake, my first line of attack was simply to cut all added salt out of my diet. That actually had only a small effect on the evening foot swelling, as shown in the following photo taken in the evening on August 15, 2021, after 1 week with no added salt:

The foot swelling is reduced but is still quite significant. You still can't see the veins and tendons of my feet, normally quite visible. For comparison, here's how my feet looked in the morning on the next day:

Even in the morning, my left foot remained somewhat swollen and although my right foot is better it is not my normal for morning.
I continued with the low-salt "meats and sweets" approach into 2022, without seeing significant progress in reducing the evening foot swelling. At that point I began to think I needed more significant dietary changes.
As a Chinese medicine physician, I knew that foot swelling and cold feet could indicate impaired kidney and cardiovascular function. On the "meats and sweets" approach my diet was still high in animal protein and cholesterol and contained significant animal fat (from dairy, beef, and eggs).
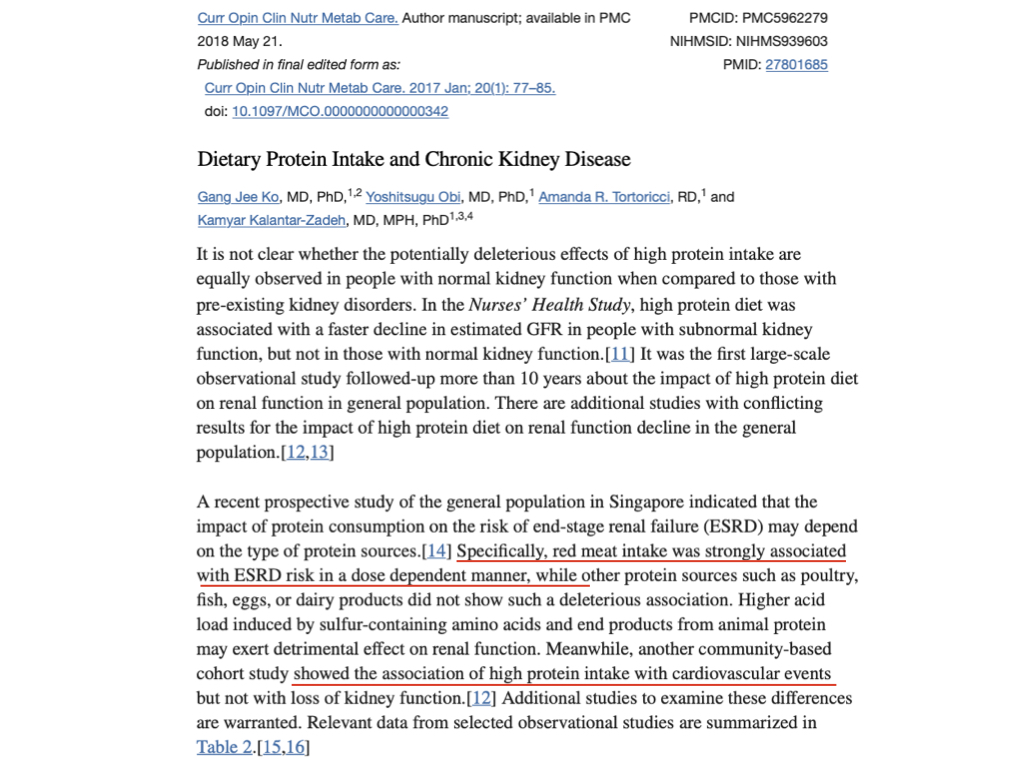
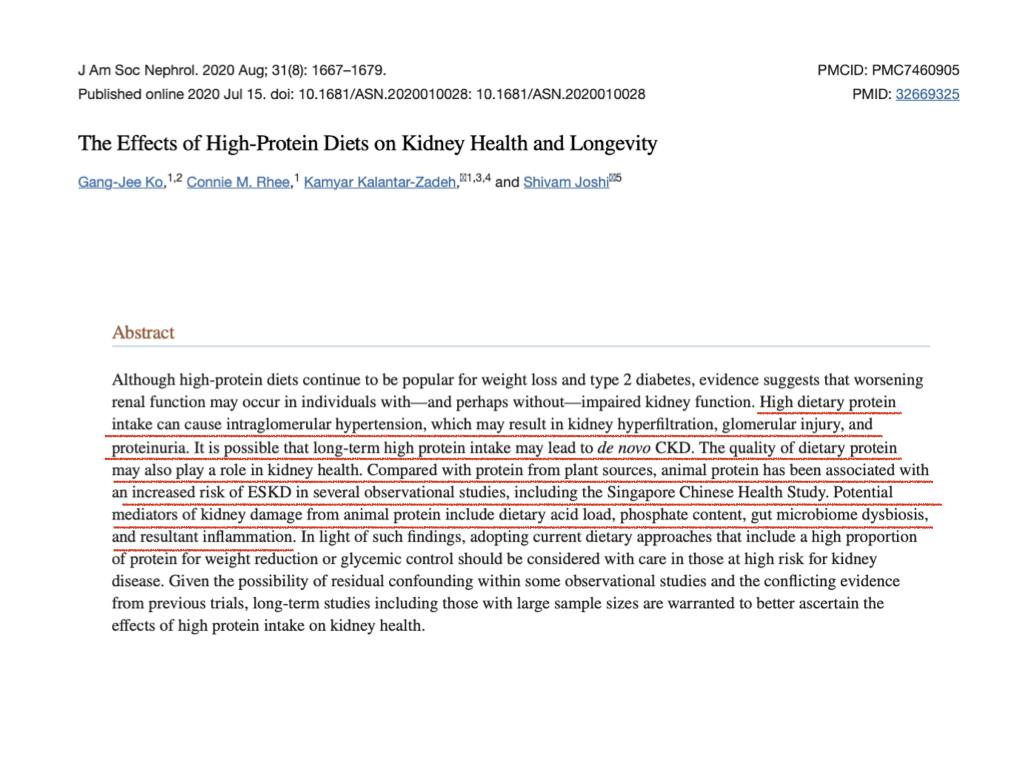
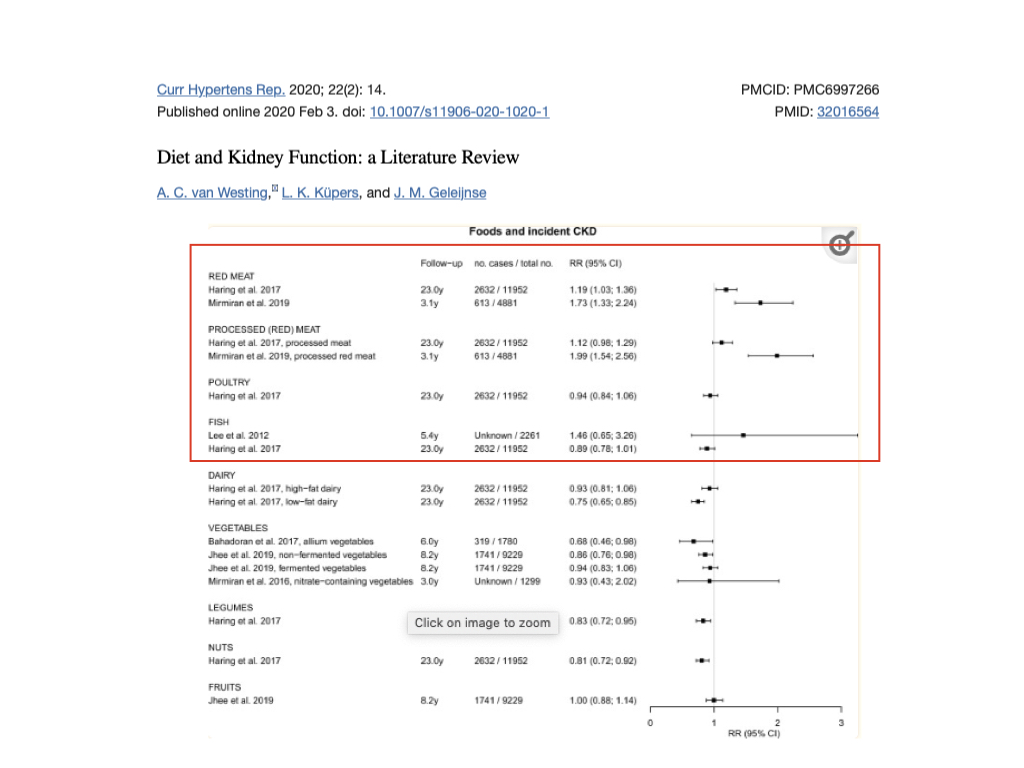
Although advocates of high protein diets claim that high protein diets do not harm the kidneys, I knew that Ellington Darden had found that a very high animal protein diet had caused his kidneys and liver to hypertrophy. I decided to look at the evidence myself. I found significant evidence that diets high in animal meat protein, particularly red meat, may impair kidney function, whereas dairy products and plants rich in protein – legumes and grains – seem to protect against loss of kidney function.
 |
 |
 |
 |
 |
 |
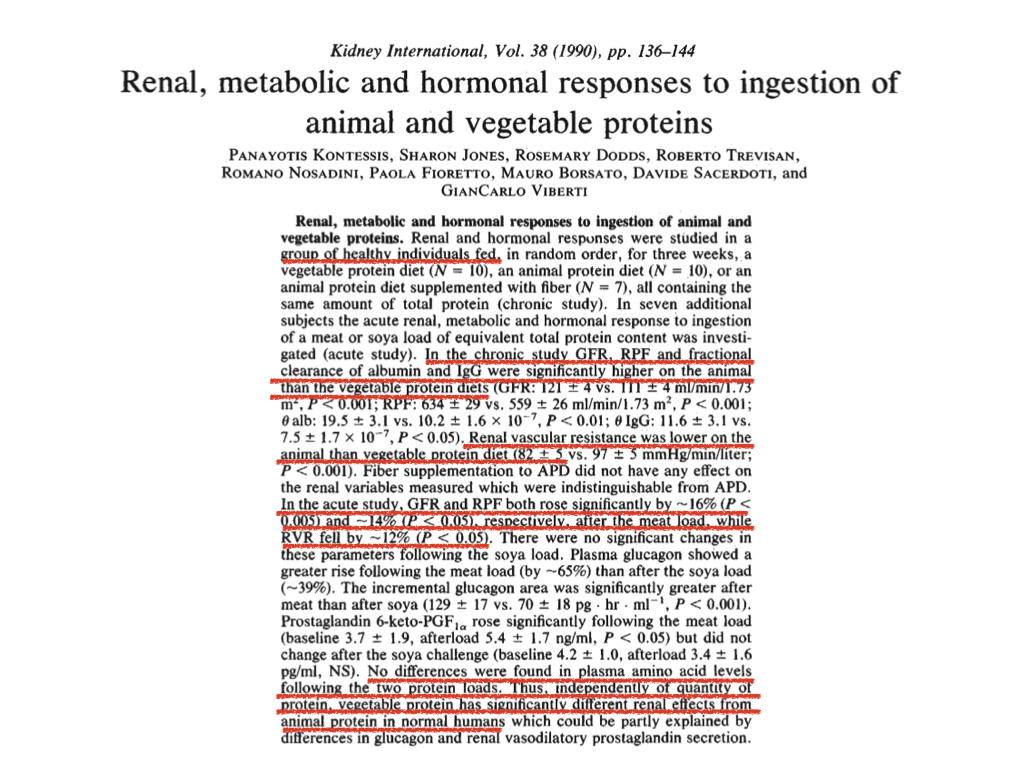
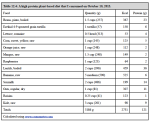
Kontessis and colleagues may have produced the strongest direct experimental evidence of the differential effects of animal and plant protein on human kidney function. For a chronic study, they had healthy subjects eat three different diets, each for 3 weeks. Each subject ate each diet in randomly determined order with one week washout between each 3 week controlled diet period. All subjects were meat-eaters by habit, so all were adapted to eating a high animal protein diet.
During the animal protein diet (APD) subjects ate a diet providing 70% of protein from animal products (only 56 g animal protein per day). During the vegetable protein diet (VPD) period subjects ate a diet providing 76 g of plant-based protein daily, with no animal protein. During the animal protein diet with fiber supplementation (APD+F) the subjects ate the 70% animal protein diet supplemented with fiber to match the fiber content of the VPD.
For an acute feeding study, they had all subjects fast, then one group (n=4) ate 80 g of protein as lean cooked beef (raw weight of ~390 g) and the other group (n=3) ate 80 g of soy protein (from 96 g of soy protein powder mixed with water and low calorie cordial as flavoring. Again, all subjects were habitual omnivores already adapted to diet providing the bulk of protein from animal sources.
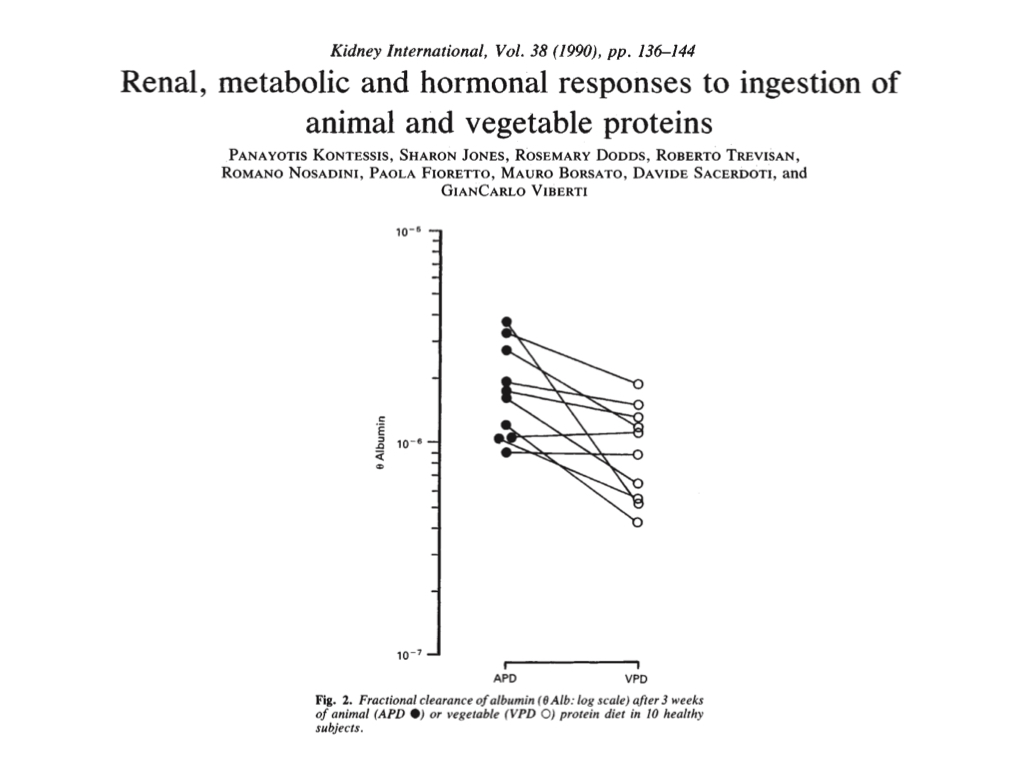
During the APD and APD+F phases, the subjects showed markers of impaired kidney function, including increased glomerular filtration and decreased renal vascular resistance. Of most concern, 8 of 10 subjects showed significantly or markedly increased urinary loss of albumin (a plasma protein that regulates tissue water levels):
During the acute feeding experiment, they found that the high (80 g) plant (soy) protein load did not increase glomerular filtration rate (GFR) or renal plasma flow (RPF), but the high (80 g) animal (beef) protein load did.
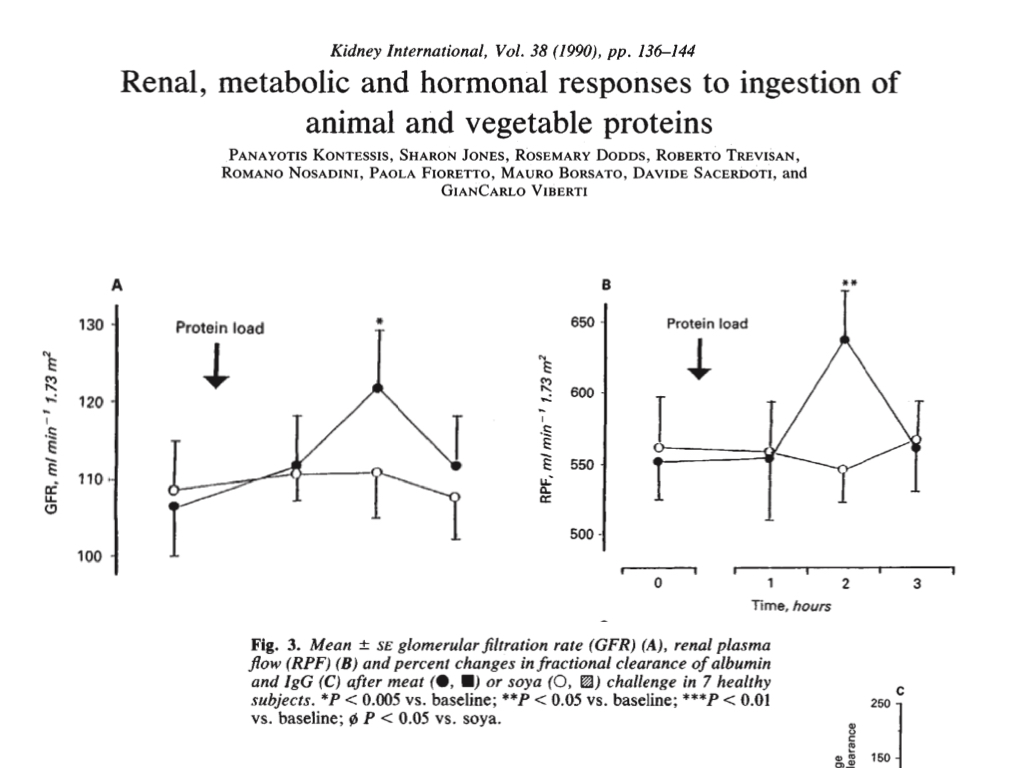
Of greater concern, the beef protein load resulted in acute loss of proteins (albumin and IgG globulin) in the urine, whereas the soy protein load caused albumin retention and a comparatively small increase in urinary globulin.
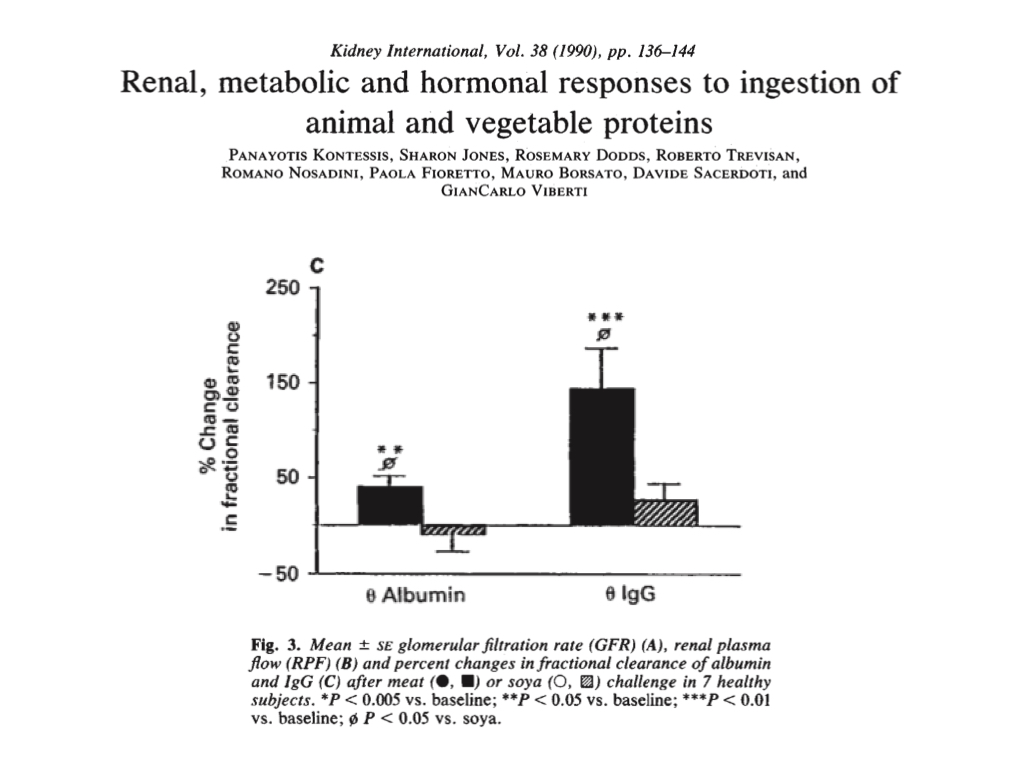
The team concluded that although the animal and plant proteins both raised plasma amino acid levels to a comparable degree in their healthy subjects, in respect of kidney function, eating the plant protein diet or meal had an effect similar to eating a low protein diet, supporting healthier kidney function.
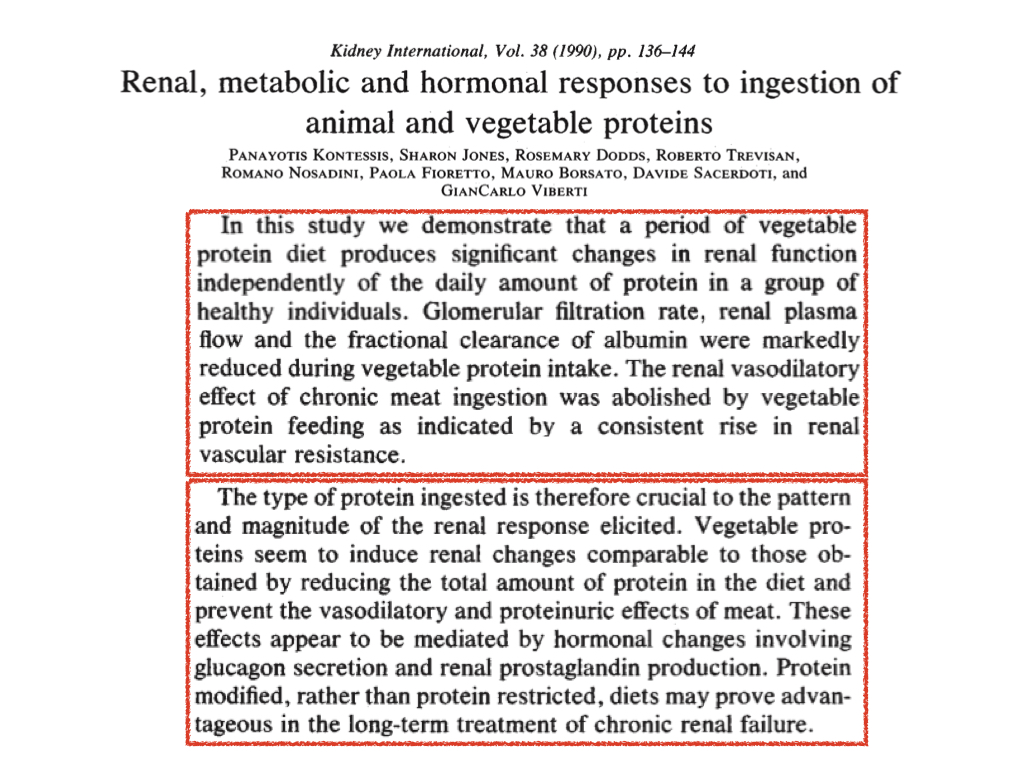
To reiterate, this study showed that, in healthy subjects, a diet containing as little as 56 g of animal protein per day markedly increased urinary loss of albumin protein, compared to diet containing no animal protein. Further, a single meal containing 80 g of protein from lean beef caused marked urinary losses of albumin and globulin in healthy subjects. This study alone provides evidence that a diet rich in animal protein can impair kidney function and induce continuous loss of plasma proteins. Further, it suggests that a plant-based diet will reduce protein requirements because less protein will be lost in the urine.
When my foot swelling problem emerged, I was eating 150-200 g of animal protein per day and 50-100 g of animal protein per meal. This study indicates that my level of protein intake could have markedly impaired my kidney function and caused me to lose plasma proteins in my urine.
Plasma proteins play a very important role in regulating tissue water levels. Plasma proteins hold water in the blood and act as "water magnets" to draw water out of tissues into the blood. About 75% of the osmotic pressure of the capillary membranes is related to albumin. Low levels of plasma proteins result in water flowing out of the blood into tissues, which causes edema such as my foot swelling. Since a high animal protein intake causes loss of plasma proteins (including albumin and globulin) in the urine, it may result in low plasma proteins and consequent edema.
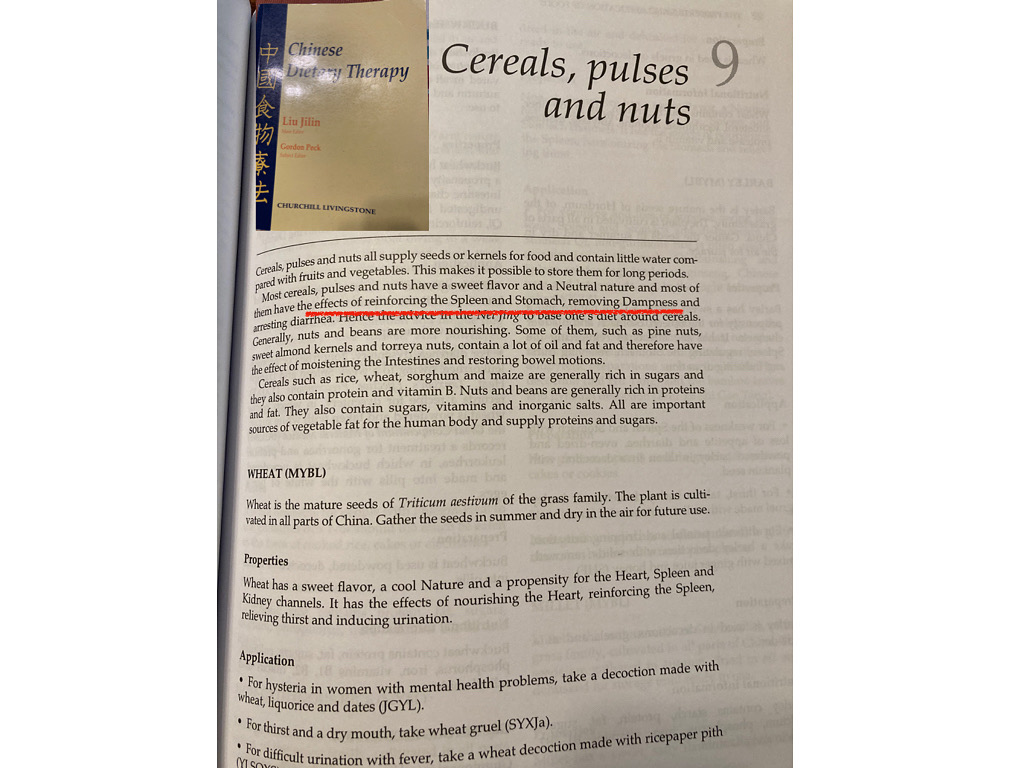
Further, Chinese medicine prescribes legumes and cereal grains to reduce edema.
|
Finally, I knew that T. Colin Campbell had noted a strong link between animal protein intake and cardiovascular disease in population and experimental studies, which he discussed in his book The China Study as well as in the American Journal of Clinical Nutrition (2000) and the Journal of Geriatric Cardiology (2017). The following photo is from the latter article: |
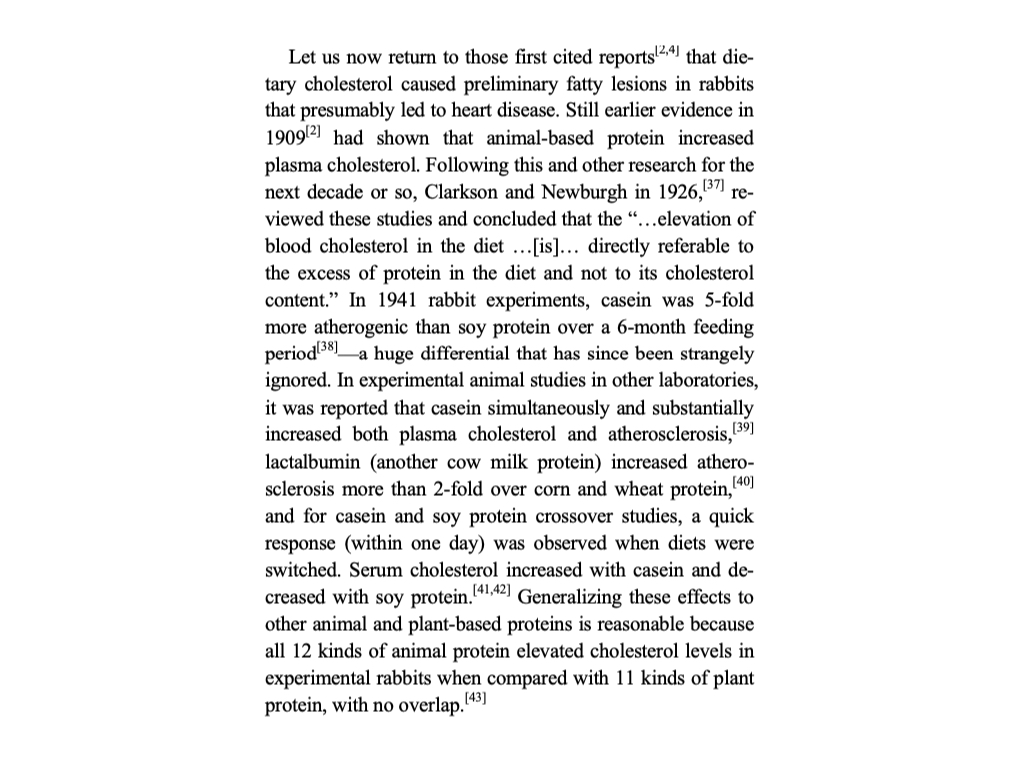
As mentioned, when I ate a hypercarnivore diet I had very high total cholesterol and LDL levels. Since oxidized LDL is a vasoconstrictor, my very high total cholesterol level on a high meat and fat diet may have contributed to reduced blood circulation to and from the extremities, resulting in cold and swollen feet.
All this suggested that my foot swelling and impaired circulation might be the consequence of eating a diet high in meat and fat and low in legumes and grains. The only way to test the hypothesis in my case was to adopt a diet with little or no meat and plenty of legumes and grains.
Although I had adopted a meat-based diet in hopes of healing my psoriasis, as I mentioned above, and discussed here, I got the best results (but not complete healing) when I restricted fatty red meat and I ate more fruit, reduced fat dairy products, and leaner beef and poultry. The literature review below found meat and fish suspects and although poultry appeared neutral, eliminating poultry and eggs would facilitate reduced animal protein and particularly sulfur amino acid intake (because eggs and poultry have very high total protein and sulfur amino acid concentrations). Since dairy product intake appeared either neutral or inversely related to kidney disease (just below the red box in the image), I decided to retain dairy products –– primarily milk and yogurt –– in my daily diet.
Deep Self-Reflection
As my search for a solution to my foot swelling led me once again to face the growing mountain of evidence indicating that diets rich in animal products promote disease in humans, I was forced to deep self-reflection. I had faced this body of evidence before, particularly when I wrote my book Powered by Plants, which involved reading the several hundred studies and books (Powered by Plants has more than 800 footnotes and a 21-page bibliography) that provided evidence for the book's thesis that humans are designed by Nature for a whole foods plant based diet.
Since writing Powered by Plants, I wrote the Hypercarnivore Diet (now out of print), in which I collected what I took to be the best evidence for the thesis that humans are designed for an animal-based diet. Thus I may be unique in having taken time and energy to deeply explore and document the evidence and arguments for both sides of this debate.
Upon comparing the two books and bodies of evidence, I concluded that the evidence available to support the idea that humans are designed for a diet composed predominantly (not necessarily exclusively) of whole plant foods far outweighs the evidence to support the idea that humans are designed for an animal-based diet, both in quantity and quality.
Thus, I had to question myself: Having known all that I wrote in Powered by Plants, how could I have deceived myself so thoroughly to have written the Hypercarnivore Diet?
This quest led to a deeper understanding of my motives for eating meat and a recovery of my philosophical-ethical senses and spiritual calling.
For 4 decades, since completing my bachelor's and master's degrees in philosophy, with a specialty in Vedic and Buddhist thought, I have practiced yoga and meditation for the purpose of having a direct experience of the Supreme Being (Ultimate Reality, God). Yoga requires the practice of ahimsa, non-harming, and according to traditional yoga masters, this requires the sincere yoga student to adopt a lactovegetarian diet.
|
In Yoga & Ayurveda: Self-Healing and Self-Realization, Dr. David Frawley, director of the American Institute of Vedic Studies explains why the yoga tradition promotes a lactovegetarian diet: "Meat-eating is something that any student of yoga should reduce, if not avoid altogether. This is particularly true of red meat. Of course, the main reason is that meat-eating violates the yogic principle of ahimsa or non-violence, which is the first of the yamas or lifestyle disciplines of yoga practice. If our yoga practice is based upon harming other creatures it cannot go far." (page 172 of paperback) |
He goes on to explain potential adverse physical, mental, moral and spiritual effects of meat-eating, such as increasing one's propensity to anger, lust, fear and other negative emotions, physical and mental inertia, violence and crime, and physical, sensory, mental, and moral insensitivity.
One may easily compare the mentality, manners and moral-spiritual orientation of advocates and followers of meat-based diets to those of advocates and followers of plant-based diets. For the most part the contrast is quite evident. One crowd is relatively brutal, concerned primarily with individual freedom, physical strength and dominance, and reveling in the materialistic sensory pleasures (e.g. eating rich fatty meat), killing animals and being 'blood-thirsty', with limited philosophical, moral and spiritual orientation, often Abrahamic in outlook, i.e. expecting and even delighting in conflict (e.g. man vs nature, man vs other animals) with zero-sum outcomes (we win, you lose). The other crowd is relatively gentle, concerned more with individual responsibility (to society and other creatures), philosophy, justice, morality, spirituality and elevating humanity above the brutes even if this requires sacrificing some sensory pleasure; this crowd has a more Dharmic outlook seeking harmony between man and nature and man and other creatures with win-win solutions.
Frawley notes, in contrast to vegan ideology, "The yoga traditions of India regard dairy products as excellent foods, particularly for individuals on the spiritual path [page 176]."
In his book Transition to Vegetarianism, Rudolf Ballentine, M.D., a yogi and former president of the Himalayan International Institute, presents the lactovegetarian diet as the middle way between meat-eating and veganism:
|
"Although a number of reasonable possibilities exist for those considering a new diet, the lactovegetarian diet seems destined to emerge as the most logical choice because it incorporates major improvements without taking them to extremes. The conventional North American meat-based diet of the mid-to-late twentieth century, and the strict vegan meatless diet, stand at either end of a continuum that encompasses much of the range of dietary habits today. |
|
"The meat-based diet is high in protein, fat, salt, phosphorus, and calories, but quite low in fiber. It is more often accompanied by tobacco, alcohol, coffee, and sugar, as well as a host of chemical additives that are prevalent in the foods that currently make up such a diet. "The vegan diet is low in protein, sometimes lower than is reassuring. It is low in phosphorus, too, which is an advantage, but it is also low in calcium. It's rich in fiber––maybe even too much so. And it may be totally devoid of vitamin B12 and vitamin D. "The lactovegetarian diet is situated comfortably between these two extremes. Protein intake is probably optimal. Fiber is present, but not in such quantities that it will tie up minerals or burden the digestive tract. Vitamin B12 and D are adequate and reliably present... [...] "The diet that results will be, in a sense, streamlined. It provides for an efficient, uncluttered metabolism and avoids the pitfalls both of excess and of deficiency. A cleanly functioning body facilitates alertness of mind. Although such a diet embodies the principle of "less is more," it's well to remember that too little is still not enough. A regimen that is overly strict in some area––for example, the omission of all animal products––can create problems that are almost mirror images of those created by a diet that is excessive. The optimal diet is base on optima, not minima. "It's often felt that the vegetarian diet allows a smaller margin of safety than a diet based on meat, but this is not true if milk products are included. A movement away from the lactovegetarian range, either into a meat diet to the left or a vegan diet on the right, will provide excesses of some nutrients, but insufficiencies of others." |
|
I first adopted a whole foods lactovegetarian diet when I was about 20 years old, while studying philosophy in college, in order to practice noble non-violence and lift my moral standard, long before I had even heard of veganism. I first read Ballentine's excellent book Diet and Nutrition: A Holistic Approach, in which he first clearly explained the advantages of the lactovegetarian diet over both meat-eating and veganism, in the early 1980s (first publication was 1978). I first read his Transition to Vegetarianism in the early 1990s, shortly after its first publication. |
If I remember correctly, after having already eaten a lacto-ovo-vegetarian diet for several years in my early 20s, I first adopted a whole foods plant based macrobiotic dairy-free diet around age 24, to see if it would improve my psoriasis. I had some improvements in my skin and allergies, but a dramatic loss of muscle and vitality (more below). That started me on a path alternating between whole foods plant based veganism (and associated nutritional deficiencies) and whole foods diets that included dairy or meat, including phases with pretty heavy meat-eating (and associated nutritional excesses), such as paleo diet and hypercarnivore.
In retrospect I believe I may have gotten caught in alternating between the vegan diet and meat-dominant diets because these extremes might dysfunctionally complement one another: Once one develops deficiencies on a vegan diet, one may be attracted to meat-eating to correct the depletion; but after a time on a meat-heavy diet, if one has previous experience with a whole foods plant based diet, one might be re-attracted to a whole foods plant based vegan diet to reduce or counterbalance the accumulation of excesses of fat, cholesterol, protein and minerals (e.g. iron) produced by a stint on a heavy meat-based diet (paleo, keto, etc.). Thus one may get caught in an unhealthy cycle of depletion (by vegan eating) followed by repletion (by meat eating) and so on. Vegan diets and meat-rich diets might present together a binary con that keeps people from adopting a traditional, proven sustainable middle path diet: lactovegetarian.
In my case, during my several early extended attempts at eating a vegan, very low fat, low protein macrobiotic diet (during my mid-20s), I lost about 20 pounds from an already lean condition (5'9", ~155 pounds), reaching about 135 pounds. Having lost a large amount of muscle mass, my body appeared to be little more than skin and bones. I was unable to continue any type of physical training in that condition. My parents and friends thought I had either lost my mind or developed some fatal disease.
Here's a photo of me taken when I was in my late 20's, during a period when I was eating a very low fat, low protein, vegan macrobiotic diet:
If I recall correctly, I weighed less than 140 pounds, during the third period when I had done a very low fat, low protein vegan diet, and this time, combined with acupuncture and herbal therapy, the effort resulted in healing of the largest psoriasis-like lesion I had at the time.
Subsequently, several times I repeated the strict low-fat, low-protein vegan diet aiming to produce further improvements in my skin. However, whenever I did I sustained the same type of weight loss and depletion, and after a sufficient period of time I found myself craving animal protein and attracted to meat-eating to rectify the loss of lean mass and vitality.
In hindsight, I would have been better off simply adding some milk back into my whole foods plant based diet, but I did not do that because I was under the influence of several critics of dairy products. Both of the leading teachers of the Japanese macrobiotic diet theory (primarily Michio Kushi and Herman Aihara) and the whole foods plant based doctors (principally John McDougall, Neal Barnard and T. Colin Campbell) had convinced me that using milk products is at least as harmful if not more harmful to health than eating meat. Further, vegan ideology argued that eating milk was morally at least as reprehensible as meat-eating, if not more so.
Later in my journey, I paid attention to advocates of pseudo-paleolithic diets (primarily Loren Cordain and Ray Audette), who also claimed that, of all possible animal products, milk is the most harmful to health because, allegedly "humans are not adapted to drinking milk." "Paleodiet" advocates continue to assert that no humans are genetically adapted to dairy products despite the fact that one of the few well-established genetic adaptations to specific foods is adult lactase persistence in Caucasians, the only function of which is to facilitate digestion of milk. I happen to be of Hungarian (50%), German, Polish, Irish and Nordic descent, and all of these nationalities exhibit high rates of lactase persistence, especially Hungarians, of whom about 80% are predicted lactase persistent.
Thus, the vegan, macrobiotic, whole foods plant based, and paleodiet ideologies all together gave me the idea that if I was going to eat any animal product I might as well eat meat in preference to dairy. But there was another root to this weed.
The Social Ordeal
From the first day I chose to adopt a lacto-ovo-vegetarian diet in my early 20s, my mom was personally offended that I would not eat the meat-based meals she cooked and she refused to learn to cook anything that I would prefer to eat when I was vegetarian or vegan. She believed she understood nutrition better than I and insisted that everyone must eat meat. My dad did not understand nor respect my choice either. Both took offense at any suggestion that meat-eating was immoral. I would not budge because it was a matter of principle for me. It became an ordeal to share meals or even visit them, because disagreements over food would adversely affect almost every visit. My mother would not prepare meals that I would eat, and they refused to eat vegetarian meals in my home.
When my father was diagnosed with prostate cancer, I told them about research by Dean Ornish and my then-friend Gordon Saxe showing that a whole foods plant based diet might help. My mom took offense at the suggestion that her cooking/eating style had contributed to my father getting cancer, and especially since neither his oncologist nor his urologist made mention of any role of animal protein in cancer promotion or recovery, my father simply refused to believe that avoiding meat could help him overcome his disease.
The conflict was painful, and caused me to doubt myself. My parents refused to budge so I could only bridge the gap, even if it meant abandoning my principles and calling. I did not realize the degree to which that painful conflict with my parents had influenced my dietary history until 2 years after they died when seeking the solution to my foot swelling.
During periods when I ate a vegan diet I also had some very stressful interactions over food and diet with other people in my familial circle. Research shows that about 15% of people who attempt a vegetarian diet eventually quit primarily because being a vegetarian in a non-vegetarian society makes social life an ordeal. Unless you have tried eating a meat-free diet in the meat-dominated culture of the U.S.A., you would not understand the social difficulties involved.
Up until this period of self-reflection that accompanied my choice to delete meat in order to correct my foot swelling problem, I did not realize (or want to accept) that I was one of the people who had found it difficult to sustain a vegetarian diet because it interfered with my social life. I wanted to think that I was motivated only by reason, evidence, and self-interest, not emotions. It was not until 2022, 2 years after my parents died, that I fully understood and acknowledged that when my parents were alive I was unconsciously motivated to find or invent a "healthy" way to eat a meat-based diet so that I could have a less strained relationship with them and other non-vegetarian members of my social circle.
This means I was unconsciously seeking a justification for or reason to eat meat. Given the power of the mind, it may also mean that I unconsciously created conditions to justify re-introducing meat into my diet. Stress, particularly stress in family relationships, promotes many stress-related diseases, which includes skin conditions like psoriasis. For example, one study reports that up to 88% of psoriasis cases report stress being a trigger for a psoriasis outbreak, and that stress reduction contributes to remission of psoriasis.
During the last year (2016) of the last period that I was eating a vegan whole foods plant based diet, I had a blood test that found slightly low levels for phosphorus (2.2 mg/dl, normal range 2.5-4.5) and globulin (1.6 g/dL, normal range 2.0-3.7). Every thing else was stellar, including total cholesterol (154 mg/dL), LDL (78 mg/dL), HDL (60 mg/dL), triglycerides (78 mg/dL), glucose (88 mg/dL).
Now I know that a slightly low phosphorus is probably a good thing, since there is a body of evidence indicating that excess dietary phosphorus promotes disordered mineral metabolism, vascular calcification, bone loss, and impaired kidney function. Aside from processed foods, meat, poultry, and eggs are the primary sources of the excess of phosphorus in the hazardous form. In contrast, whole plant foods provide phytate which has preventive and therapeutic actions against cancer, diabetes, atherosclerosis, coronary artery disease, kidney stones, and heavy metal toxicity. Not surprisingly, my serum phosphorus level did rise after I adopted a hypercarnivore meat-based diet in 2017, but so did my total cholesterol (reached 419 mg/dL), LDL (reached 293 mg/dL), and fasting glucose (reached 103 mg/dL), none of these being good signs, though I rationalized them as "dawn phenomenon" and "lean mass hyper-responder" numbers instead of realizing that I was making myself insulin resistant with a high saturated fat diet.
As for the low globulin, it could have been due to a slightly suboptimal protein nutrition, although that is questionable since my albumin was excellent (4.7 g/DL, normal range 3.3-4.9). It could have just been a lab measurement error; I don't know because I did not order a retest right away, which would have been a good idea, since I was in general good health and had no reason to suspect that this low globulin level could be kidney or liver disease at the time.
My globulin did improve to normal range in the first labs I had done about 6-8 months after adding meats back to my diet. Unfortunately, I did not try just adding a couple of cups of milk into my otherwise whole foods plant based diet, using a minimal effective dose approach. That's my point. In the mental state I was in due to enduring repeated and continuing social conflicts centered on my meat-free diet, I took the slightly low phosphorus and globulin as "signs" that I was significantly malnourished on the vegan diet, getting insufficient phosphorus and protein, and "needed" to shift to obtaining most or all of my protein from meat. In hindsight I see that I was subconsciously waiting and looking for some reason to resume eating meat, to get myself out of the dietary conflict with my parents and others.
Over the past 40+ years (since I first adopted a lactovegetarian diet), I chose to eat a lactovegetarian or vegan (often macrobiotic) diet when I was following my heart and chosen moral-spiritual path. Alternatively, I chose to eat meat (with or without dairy) when I had strong cravings after a long period of eating a vegan diet, or when I found some reason to believe that eating meat would improve my skin health, and I now realize that after sufficient periods of time on a vegan diet, I was also driven to eat meat by a desire to find some way to bridge the uncomfortable gap that existed between myself and my meat-eating parents (and other meat-eaters in my social circle) whenever I was eating a meat-free diet.
Now, after giving meat-based diets a more than fair chance to improve my health, and finding that they did not fully resolve my psoriasis, but involved several unpleasant and potentially lethal complications (hypercholesterolemia, cholestasis/fat indigestion, cramping, foot swelling, impaired circulation), I am at the point where I can no longer give meat-eating the benefit of the doubt in regards to health effects. I no longer have an unconscious influence or conscious reason to sacrifice my moral and spiritual calling, principles and progress in order to create a fragile resonance with my parents.
Resolution of Foot Swelling
By late May of 2022, I understood that the scientific evidence presented above suggested that my kidney (and heart) functions would likely improve only if I adopted a moderate protein whole foods lactovegetarian diet; in turn, improved kidney and heart function could reduce or eliminate the foot swelling.
So, I did it. I dropped meat from my diet entirely starting that summer. I ate grains, legumes (including soy milk and tofu), vegetables, fruits, nuts, seeds, and included no more than 2 cups of milk or yogurt most days, only occasionally taking 3 cups. I ate eggs in some baked goods or only very occasionally as a stand-alone dish.
My total protein intake declined from a typical 120-160 grams daily, mostly from animal protein (dairy and meat) on the meats and sweets regime, to 80-100 grams daily, mostly from legumes and grains, with only 16 grams of that total coming from milk or yogurt on most days. That means 75-80 percent of my protein came from plants on a daily basis.
This solved the problem.
The two photos below were taken almost exactly one year apart, both after 9 PM and both on Sundays when I spent the entire afternoon sedentary, deterred from outdoor physical activity by high temperatures and humidity with a high heat index in lower Michigan.
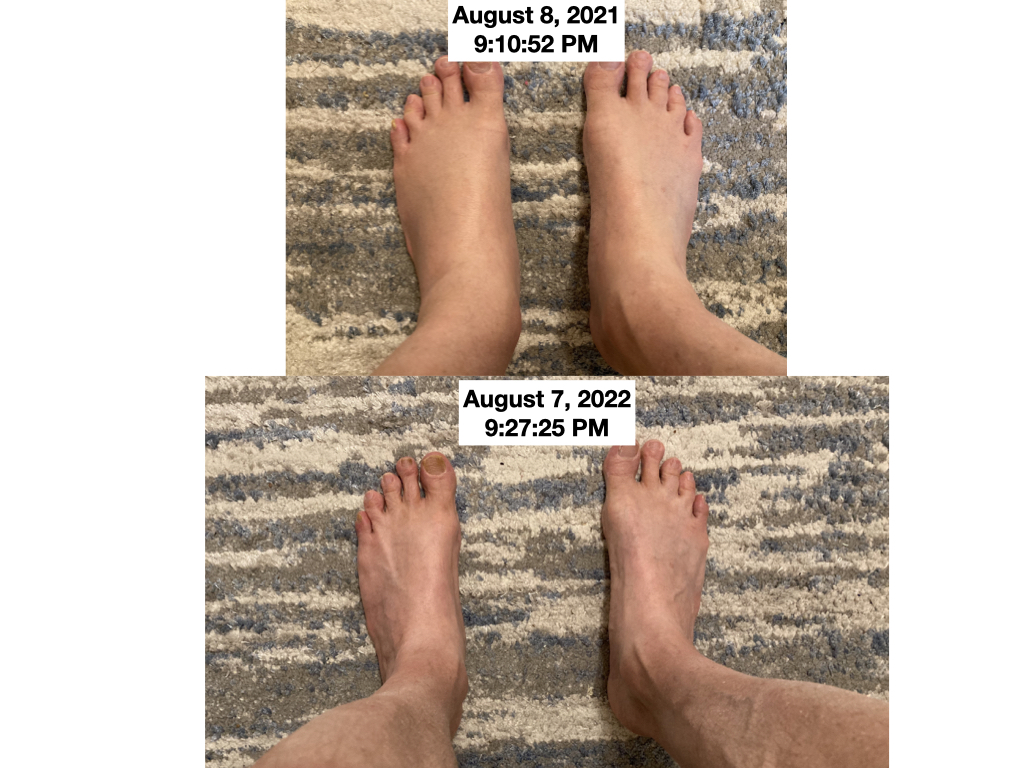
By August of 2022, I no longer suffered from evening foot swelling (lower limb edema), not even on very humid days when I was sedentary most of the day. Below, compare the upper photo from the evening of August 8, 2022, about 2 months after adopting a low animal protein, moderate total protein diet, with the photo below from the morning of August 16, 2021, when I was still on a high animal protein diet.


After adopting the low animal protein, moderate total protein whole foods lactovegetarian diet, my feet in the evening look similar to if not better than how they looked only in the morning a year before when I was eating a high animal protein diet with no added salt.
Below is a photo of my feet taken in the morning on August 12, 2022, to compare with the previous morning photo from August 16, 2021.

You can see how the veins and tendons were more prominent on the morning of August 12, 2022, after about 2 months on a lactovegetarian diet, than the morning of August 16, 2021, when I was on a no-salt added, high animal protein "meats and sweets" diet. The circulation to my feet improved markedly by adopting a low fat, moderate protein lactovegetarian diet.
I am very happy with the result achieved by removing meat from my diet and expect the improvement to continue as my kidney and cardiovascular functions improve.
In summary: I fixed my foot swelling problem by deleting meat and eating a low sodium, whole foods lactovegetarian diet.
Recent Articles
-
Ancient Roman Soldier Diet
Apr 14, 25 05:19 PM
A discussion of the ancient Roman soldier diet, its staple foods and nutritional value, and a vegan minimalist version. -
High Protein Chocolate Tofu Pudding
Jul 01, 24 12:41 PM
A delicious high protein chocolate tofu pudding. -
Vegan Macrobiotic Diet For Psoriasis
Sep 05, 23 06:36 PM
Vegan macrobiotic diet for psoriasis. My progress healing psoriasis with a vegan macrobiotic diet. -
How Every Disease Develops
Aug 04, 23 06:22 PM
How every disease develops over time, according to macrobiotic medicine. -
Why Do People Quit Being Vegan?
Jun 28, 23 08:04 PM
Why do people quit being vegan? How peer pressure and ego conspire against vegans. -
Powered By Plants
Mar 16, 23 08:01 PM
Powered By Plants is a book in which I have presented a lot of scientific evidence that humans are designed by Nature for a whole foods plant-based diet. -
Carnism Versus Libertarianism
Dec 30, 22 01:55 PM
Carnism Versus Libertarianism is an e-book demonstrating that carnism is in principle incompatible with libertarianism, voluntaryism, and anarchism. -
The Most Dangerous Superstition Book Review
Nov 15, 22 08:46 PM
Review of the book The Most Dangerous Superstition by Larken Rose.